For years, scientists have warned that bird flu - better known as H5N1 - could one day make the dangerous leap from birds to humans and trigger a global health crisis.
Avian flu - a type of influenza - is entrenched across South and South-East Asia and has occasionally infected humans since emerging in China in the late 1990s. From 2003 to August 2025, the World Health Organization (WHO) has reported 990 human H5N1 cases across 25 countries, including 475 deaths - a 48% fatality rate.
In the US alone, the virus has struck more than 180 million birds, spread to over 1,000 dairy herds in 18 states, and infected at least 70 people - mostly farmworkers - causing several hospitalisations and one death. In January, three tigers and a leopard died at a wildlife rescue centre in India's Nagpur city from the virus that typically infects birds.
Symptoms in humans mimic a severe flu: high fever, cough, sore throat, muscle aches, and, at times, conjunctivitis. Some people have no symptoms at all. The risk to humans remains low, but authorities are watching H5N1 closely for any shift that could make it spread more easily.
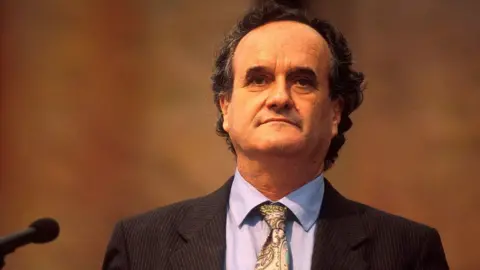
That concern is what prompted new peer-reviewed modelling by Indian researchers Philip Cherian and Gautam Menon of Ashoka University, which simulates how an H5N1 outbreak might unfold in humans and what early interventions could stop it before it spreads.
In other words, the model published in the BMC Public Health journal uses real-world data and computer simulations to play out how an outbreak might spread in real life.
The threat of an H5N1 pandemic in humans is a genuine one, but we can hope to forestall it through better surveillance and a more nimble public-health response, Prof Menon told the BBC.
A bird flu pandemic, researchers say, would begin quietly: a single infected bird passing the virus to a human - most likely a farmer, market worker, or someone handling poultry. From there, the danger lies not in that first infection but in what happens next: sustained human-to-human transmission.
Because real outbreaks start with limited, messy data, the researchers turned to BharatSim, an open-source simulation platform originally built for Covid-19 modelling, but versatile enough to study other diseases.
The key takeaway for policymakers is how narrow the window for action can be before an outbreak spirals out of control, the researchers say. The paper estimates that once cases rise beyond roughly two to 10, the disease is likely to spread beyond primary and secondary contacts.
To keep the study grounded in real-world conditions, the researchers chose a model of a single village in Namakkal district, Tamil Nadu - the heart of India's poultry belt.
Namakkal is home to more than 1,600 poultry farms and some 70 million chickens; it produces over 60 million eggs a day.
The simulations also highlighted an awkward trade-off. Quarantine, introduced too early, keeps families together for long stretches - and increases the chance that infected individuals will pass the virus to those they live with. However, if introduced too late, it does little to slow the outbreak.
This approach comes with caveats. The model relies on one synthetic village, with fixed household sizes and daily movement patterns. Without accounting for simultaneous outbreaks seeded by migratory birds or behavioral shifts after knowing about birds dying, the model might not capture the full complexity of a real outbreak.
With refinements and updates as data comes in, the simulations could provide public health officials invaluable insight in the early hours of an outbreak, highlighting which actions matter most before the containment window closes.